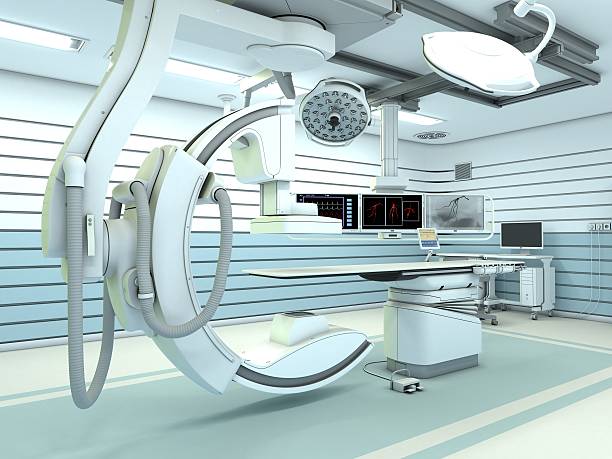
What is Interventional Radiology?
Interventional Radiology (IR) is a specialized medical field that uses advanced imaging guidance to perform minimally invasive diagnostic and therapeutic procedures. This innovative approach allows interventional radiologists—highly trained medical doctors—to treat various conditions without traditional surgery, leading to faster recovery times and reduced risks for patients.
Key Aspects of Interventional Radiology
Advanced Imaging Guidance
Interventional radiologists use state-of-the-art imaging technologies to precisely guide procedures in real time, including:
✔ Fluoroscopy – Continuous X-ray imaging for dynamic visualization.
✔ Ultrasound – Real-time imaging without radiation exposure.
✔ Computed Tomography (CT) – High-resolution cross-sectional imaging.
Minimally Invasive Procedures
A hallmark of IR is the use of tiny incisions or natural body openings to access and treat affected areas. These techniques result in:
✅ Less pain and discomfort compared to traditional surgery.
✅ Faster recovery and shorter hospital stays.
✅ Reduced risk of complications.
Therapeutic Interventions
Interventional Radiology offers cutting-edge treatments for various medical conditions, including:
- Angioplasty & Stenting – Widening and supporting narrowed blood vessels.
- Embolization – Blocking blood vessels to stop bleeding or shrink tumors.
- Radiofrequency Ablation (RFA) – Using heat to destroy tumors or abnormal tissues.
- Catheter-Based Therapies – Delivering medications or targeted treatments through thin tubes (catheters).
Diagnostic Interventions
IR is also instrumental in diagnosing conditions through minimally invasive sampling and drainage techniques, such as:
- Biopsies – Extracting tissue samples for analysis.
- Fluid Drainage – Removing excess fluid from organs or infected areas.
Vascular & Non-Vascular Interventions
Interventional radiologists specialize in both vascular (blood vessel-related) and non-vascular (organ-related) procedures, ensuring comprehensive care for a wide range of conditions.
Collaborative & Patient-Centered Care
IR specialists work closely with other medical professionals, including surgeons, oncologists, and primary care physicians, to provide personalized treatment plans tailored to each patient’s needs.
Outpatient & Inpatient Procedures
- Many IR procedures can be performed on an outpatient basis, eliminating the need for hospital stays.
- More complex cases may require inpatient care for close monitoring.
Technological Advancements in IR
The field of Interventional Radiology continues to evolve with innovations such as:
🚀 Robotic-assisted procedures for enhanced precision.
📡 Real-time 3D imaging for better treatment accuracy.
💡 Minimally invasive cancer treatments that reduce the need for surgery.
The Future of Interventional Radiology
Interventional Radiology is revolutionizing modern medicine by providing safer, less invasive alternatives to traditional surgery. As technology advances, IR continues to expand treatment options, improve patient outcomes, and play a crucial role across multiple medical specialties.
Patient Information
Biopsy & FNAC
What is a Biopsy?
A biopsy is a medical procedure in which a small tissue sample is removed from the body for examination under a microscope. It helps in diagnosing various conditions, including infections, inflammatory diseases, and cancer.
What is FNAC?
Fine Needle Aspiration Cytology (FNAC) is a type of biopsy that uses a thin, hollow needle to extract a small sample of cells from a suspicious area for analysis. It is a quick, minimally invasive procedure commonly used to evaluate lumps or abnormal masses.
Purpose of Biopsy & FNAC
✔ Diagnosis: Helps determine the nature of an abnormality detected through imaging.
✔ Cancer Staging: If malignancy is confirmed, a biopsy helps assess the stage and extent of cancer.
✔ Treatment Planning: Biopsy results guide healthcare providers in developing appropriate treatment strategies.
Patient Preparation
🩺 Explanation: Your doctor will explain the procedure, its purpose, and any potential risks.
📝 Consent: You will be asked to provide informed consent before the procedure.
🍽 Fasting: Follow any fasting instructions given by your healthcare team.
During the Procedure
📌 Positioning: You will be positioned appropriately to ensure accuracy and comfort.
💉 Local Anesthesia: A numbing agent may be applied to minimize discomfort.
🔬 Needle Insertion: A thin needle is inserted into the target area to collect the required tissue or cell sample.
After the Procedure
👀 Observation: You may be monitored for a short period to check for any immediate complications.
🏃 Activity: Most patients can resume normal activities shortly after the procedure.
Results & Follow-Up
📅 Timing: The time required to receive results may vary. Your doctor will discuss the findings and next steps with you.
Risks & Considerations
⚠ Bleeding & Infection: Though rare, minor bleeding or infection at the biopsy site may occur.
⚡ Mild Discomfort: Some patients may experience slight pain or bruising at the procedure site.
Biopsy and FNAC are safe and effective diagnostic tools that play a crucial role in early detection and treatment planning. If you have any concerns, consult your healthcare provider for guidance.
Pigtail Catheter Drainage: Procedure & Patient Guide
A pigtail catheter is a thin, flexible tube used to drain fluid or air from body cavities. It is commonly used for conditions such as pleural effusions, peritoneal effusions, or abscess drainage. The procedure is minimally invasive and performed under imaging guidance to ensure accuracy.
Before the Procedure
1. Patient Information & Consent
✔ The patient will be informed about the procedure, its purpose, and any potential risks.
✔ Informed consent must be obtained before proceeding.
✔ The patient should inform the healthcare provider of any allergies, medications, or underlying medical conditions.
2. Preparation
✔ Follow any specific pre-procedure fasting or preparation instructions provided by the healthcare provider.
During the Procedure
1. Sterile Technique
✔ The procedure is performed under strict sterile conditions to minimize infection risk.
✔ The healthcare provider will use aseptic techniques throughout the procedure.
2. Local Anesthesia
✔ A local anesthetic may be administered to numb the area, ensuring minimal discomfort.
3. Catheter Insertion
✔ The pigtail catheter is carefully inserted into the targeted body cavity using imaging guidance (ultrasound, CT scan, or fluoroscopy) to ensure precise placement.
4. Confirmation
✔ Imaging may be used to verify the catheter’s correct placement before beginning drainage.
After the Procedure
1. Monitoring
✔ The patient will be monitored for any complications such as pain, bleeding, or infection.
✔ Vital signs and catheter function will be observed closely.
2. Drainage Management
✔ If fluid or air drainage is required, the catheter will be connected to a drainage bag.
✔ The healthcare team will provide specific instructions on drainage care, emptying the bag, and hygiene maintenance.
A pigtail catheter is a safe and effective method for fluid and air drainage, providing relief from discomfort and aiding in recovery. If you experience pain, fever, redness, or unusual drainage, contact your healthcare provider immediately.
Guided Intra Articular Injection
Platelet-Rich Plasma (PRP) injections are an advanced treatment for osteoarthritis (OA), aimed at stimulating natural healing, reducing inflammation, and relieving joint pain. PRP therapy may help delay the need for joint surgery, such as a joint replacement, making it a valuable option for managing OA symptoms.
Before the Procedure
1. Patient Information & Consent
✔ The procedure, benefits, and potential risks will be discussed with the healthcare provider.
✔ Informed consent must be obtained before proceeding.
✔ Patients should inform their doctor about any allergies, medications, or medical conditions.
2. Preparation
✔ Follow any pre-procedure instructions, which may include fasting or medication adjustments as advised by the healthcare provider.
During the Procedure
1. Blood Collection
✔ A small amount of the patient’s blood is drawn, similar to a routine blood test.
2. Centrifugation
✔ The collected blood is processed in a centrifuge, separating the platelet-rich plasma (PRP) from other blood components.
3. PRP Injection
✔ The PRP is injected into the affected joint using imaging guidance (ultrasound or fluoroscopy) to ensure precise placement.
4. Confirmation
✔ Imaging techniques are used to verify the accuracy of the PRP injection.
After the Procedure
1. Monitoring
✔ The patient is observed for a short period to check for any immediate reactions or side effects.
2. Activity Restrictions
✔ The healthcare provider may recommend temporary activity restrictions to promote optimal healing.
3. Pain Management
✔ Pain relief medications may be prescribed if necessary.
✔ Patients should follow the prescribed medication regimen and report any unusual pain or discomfort.
PRP therapy is a safe and minimally invasive option for managing osteoarthritis, offering potential pain relief and improved joint function. If you have any concerns, consult your healthcare provider for further guidance.
AVMs Sclerosant Injection
Sclerosant injection is a minimally invasive procedure used to treat arteriovenous malformations (AVMs). It works by inducing sclerosis (scarring) in abnormal blood vessels, leading to their closure and reduced blood flow to the affected area.
Before the Procedure
1. Patient Information & Consent
✔ The procedure, its benefits and potential risks, will be discussed with the healthcare provider.
✔ Patients must provide informed consent before proceeding.
✔ Inform the doctor about any allergies, medications, or existing medical conditions.
2. Imaging Studies
✔ Imaging tests (such as ultrasound, CT, or MRI) may be performed to assess the AVM and plan the procedure.
During the Procedure
1. Local Anesthesia
✔ A local anesthetic may be applied to numb the area where the injection will be administered.
2. Catheter Placement
✔ A thin catheter is inserted into the blood vessels leading to the AVM using imaging guidance for precise placement.
3. Sclerosant Injection
✔ A sclerosing agent is injected through the catheter, causing the abnormal vessels to harden and close off.
4. Confirmation
✔ Imaging techniques may be used to verify the accuracy of the injection and assess AVM closure.
After the Procedure
1. Monitoring
✔ The patient is monitored for a short period to check for any immediate side effects or complications.
2. Activity Restrictions
✔ The healthcare provider may recommend limiting certain activities to support healing.
3. Pain Management
✔ Pain relief medications may be prescribed if needed.
✔ Patients should follow all medical instructions and report any unusual pain or discomfort.
Sclerosant injection is an effective, image-guided treatment for AVMs, offering a minimally invasive alternative to surgery. If you have any concerns, consult your healthcare provider for further guidance.
